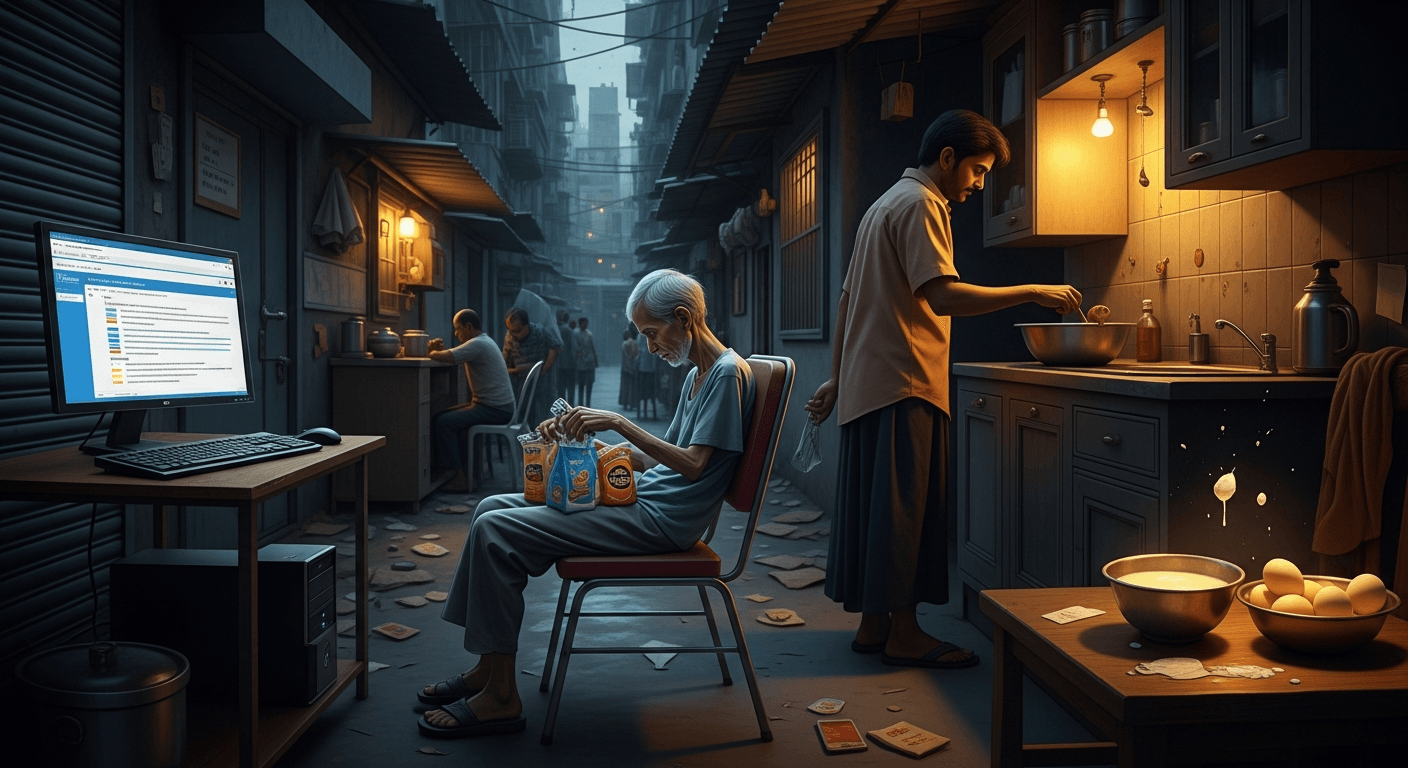
I write this as someone who has watched public-health promises land — sometimes slowly, sometimes not at all — on the thin kitchen tables of families battling tuberculosis. The Times of India piece that inspired these reflections lays out a hard truth: cash meant for nutrition arrives late or not at all, and people on long TB regimens pay with their bodies and livelihoods Broken promises: As govt delays cash transfers, hunger comes for TB patients.
I have written before about nutrition, digital tracking and last-mile delivery — ideas I described under names such as BANMALI and Poshan Tracker when urging better use of simple technology to protect the vulnerable BANMALI arrives : Named as Poshan Tracker. Those pieces were driven by the same conviction: nutrition is not an optional add-on to clinical care; it is treatment.
Why nutrition matters in TB care
- TB treatment is long and metabolically costly: standard drug-sensitive TB takes six months; drug-resistant forms can extend to 18–24 months (though newer regimens shorten some DR-TB courses to 6–9 months in certain patients).
- Undernutrition reduces drug tolerance, immune function and recovery. Trials such as the RATIONS study informed WHO guidance by showing that macronutrient support improves outcomes.
- Even modest monthly cash — intended for food — can mean the difference between two eggs and none, milk and a cup of tea, or skipping protein entirely.
What the scheme promises — and what it actually does
The Nikshay Poshan Yojana (NPY) is the government DBT (direct benefit transfer) that provides cash support to notified TB patients. It began at about ₹500/month and was raised to ₹1,000/month in recent policy decisions; energy-dense supplements for underweight patients and household-level mitigation under Ni-kshay Mitra were also announced at national level Press release: Nutritional Support to TB Patients and their Families (PIB) (estimates based on official announcements).
But implementation has repeatedly lagged. Studies and audits (including mixed-methods field work) found:
- Delays between diagnosis and first payment often measure in months rather than days; median first-payment delays of several months were reported in early assessments BMJ Open; mixed-methods DBT study (estimate: median delay ~3–5 months in some cohorts).
- Coverage gaps: not every diagnosed patient receives payments; some districts report substantial fractions unpaid (estimates vary by site; the Times of India report cited thousands unpaid in Mumbai in one recent period).
- Operational hurdles: Aadhaar seeding, lack of bank accounts, wrong or changed bank details, PFMS and NIKSHAY integration issues, and bulk/periodic processing create bottlenecks.
Human stories (composite, unnamed)
These are composite stories assembled from patterns I’ve read and heard in clinical reports and journalism — not individual interviews.
- A woman in a cramped Govandi room, recently started on DR-TB drugs, told a clinic worker she used the family’s ₹1,000 promise in her head to imagine buying milk for her toddler. Months passed; the transfer came twice in the year, in lump sums. Nutrition suffered; energy fell; clinic visits became harder.
- A young man who had to change his bank account while on treatment stopped receiving the cash after the paperwork lagged. He missed doses when hunger and physical weakness made adherence impossible.
Voices from the field (composite / unnamed)
- “We tell patients the money will reach them, but we cannot promise when,” said an unnamed TB clinic worker (composite). The frustration is real — health staff spend time chasing approvals rather than providing counselling.
- “Nutrition is treatment — not a perk,” said an unnamed NGO volunteer (composite). “When transfers falter, the clinical gains of free drugs are eroded by food insecurity.”
Mechanics of the delay: a practical breakdown
- Identification and registration: NIKSHAY registration requires accurate IDs and bank details. Many patients are migrants or informal workers with incomplete documentation. (estimate: a non-trivial fraction of urban poor lack fully seeded accounts at diagnosis).
- Systems integration and processing: Payments move from NIKSHAY to PFMS, with checks at multiple levels. Bulk processing cycles and periodic approvals can create weeks-to-months delays.
- Bank-account churn and corrections: When patients change accounts, update errors or mismatches in Aadhaar linkage can stall payments.
- Technology and staffing: Overburdened TB officers, poor connectivity at peripheral sites and occasional glitches in digital portals slow approvals.
Consequences for adherence and outcomes
Delays or absence of nutrition support are not just indignities; they translate into measurable risks:
- Poor adherence: undernourished patients are more likely to miss doses, lapse into treatment interruption and suffer side effects.
- Disease progression: weaker immunity and worse tolerance to drugs can push patients toward more severe or drug-resistant disease.
- Economic catastrophe: families already losing wages to illness face transport, nutritional and caregiving costs — cash meant to offset catastrophic expenditure fails when it’s delayed.
What has worked — and what we should scale
- Conditional food baskets: where NGOs or Ni-kshay Mitra donors provide food baskets, families report immediate relief. However, coverage is patchy and often dependent on local champions.
- Simpler payment triggers: immediate first instalment on diagnosis (rather than waiting for two months of adherence) reduces the critical early gap. The BMJ and operational commentaries suggest frontloading the first transfer.
- Flexible identity rules: allowing transfers to verified family accounts temporarily (with patient consent) reduces the bank-account barrier.
Policy recommendations I stand behind
- Frontload a first emergency payment at diagnosis (even a modest lump sum) so the earliest nutritional deficit is eased. This could be an automated trigger in NIKSHAY.
- Allow temporary transfers to verified family accounts (with patient consent) and streamline Aadhaar-bank seeding through field-level facilitation drives.
- Set a maximum processing-time guarantee (e.g., first payment within 7–14 days of notification) and publish district-level dashboards for accountability.
- Combine cash with in-kind options: community-managed food baskets for those who prefer or need immediate tangible support; energy-dense supplements for BMI<18.5.
- Invest in human capacity: hire/retain TB-field support staff to do last-mile verification and to assist patients with bank documentation.
- Partner transparently with civil society and CSR donors (Ni-kshay Mitra operational scale-up) to plug gaps while systems stabilize.
A call to action for readers and NGOs
- If you can donate time or funds, join or support local Ni-kshay Mitra drives that create reliable food-basket pipelines to TB patients.
- Pressure matters: ask elected representatives and local health officers for transparency on NPY disbursals in your ward — public dashboards make a difference.
- Volunteer skills: NGOs often need helped with bank onboarding drives, digital literacy sessions, and accompaniment for patients to open or correct accounts.
A final, human note
I am blunt because lives are at stake. TB is not a problem that a clinic alone can solve: it demands social protection, predictable cash or food support, and functioning last-mile systems. The money the state has promised is not charity; it is an essential part of medical treatment. When transfers fail, the clinical promise of a cure becomes hollow.
We can fix these gaps with modest design changes, more staff, and political will. Until then, those with TB — already weakened by disease and stigma — will be the canaries in our public-health coal mine.
Regards,
Hemen Parekh
Any questions / doubts / clarifications regarding this blog? Just ask (by typing or talking) my Virtual Avatar on the website embedded below. Then "Share" that to your friend on WhatsApp.
Get correct answer to any question asked by Shri Amitabh Bachchan on Kaun Banega Crorepati, faster than any contestant
Hello Candidates :
- For UPSC – IAS – IPS – IFS etc., exams, you must prepare to answer, essay type questions which test your General Knowledge / Sensitivity of current events
- If you have read this blog carefully , you should be able to answer the following question:
- Need help ? No problem . Following are two AI AGENTS where we have PRE-LOADED this question in their respective Question Boxes . All that you have to do is just click SUBMIT
- www.HemenParekh.ai { a SLM , powered by my own Digital Content of more than 50,000 + documents, written by me over past 60 years of my professional career }
- www.IndiaAGI.ai { a consortium of 3 LLMs which debate and deliver a CONSENSUS answer – and each gives its own answer as well ! }
- It is up to you to decide which answer is more comprehensive / nuanced ( For sheer amazement, click both SUBMIT buttons quickly, one after another ) Then share any answer with yourself / your friends ( using WhatsApp / Email ). Nothing stops you from submitting ( just copy / paste from your resource ), all those questions from last year’s UPSC exam paper as well !
- May be there are other online resources which too provide you answers to UPSC “ General Knowledge “ questions but only I provide you in 26 languages !






No comments:
Post a Comment